Chronic Persistent Lung Infections
Can I Get Social Security Disability Benefits for Chronic Persistent Lung Infections?
- About Chronic Persistent Lung Infections and Disability
- How to Get Disability Benefits for Chronic Persistent Lung Infections by Meeting a Listing
- Residual Functional Capacity Assessment for Chronic Persistent Lung Infections
- Getting Your Doctor’s Medical Opinion About What You Can Still Do
If you have a chronic persistent lung infection, Social Security disability benefits may be available. To determine whether you are disabled by your chronic persistent lung infection, the Social Security Administration first considers whether it is severe enough to meet or equal a listing at Step 3 of the Sequential Evaluation Process. See How to Get Disability Benefits for Chronic Persistent Lung Infections by Meeting a Listing. If you meet or equal a listing because of your chronic persistent lung infection, you are considered disabled. If your chronic persistent lung infection is not severe enough to equal or meet a listing, the Social Security Administration must assess your residual functional capacity (RFC) (the work you can still do, despite the chronic persistent lung infection), to determine whether you qualify for disability benefits at Step 4 and Step 5 of the Sequential Evaluation Process.
About Chronic Persistent Lung Infections and Disability
Chronic persistent lung infections damage lung tissue and could result in some degree of restrictive impairment. These infections can be bacterial (including mycobacterial), fungal (including mycotic), viral, or parasitic. See Residual Functional Capacity Assessment for Chronic Persistent Lung Infections.
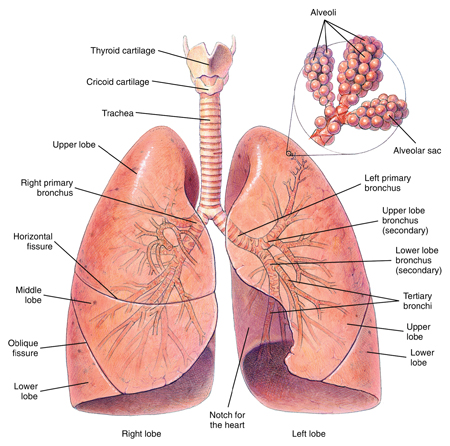
Respiratory System
Causes/Forms of Chronic Persistent Lung Infections
Mycobacterial Infections
Mycobacteria are any number of bacteria that are a part of the genus called Mycobacteria. Mycobacterium tuberculosis is the most important species in regard to human infection and is the cause of TB. There are many other species of Mycobacteria such as M. kansasii; these are less likely than M. tuberculosis to infect humans. When human infection does occur, they are frequently referred to as “atypical TB” and are a greater risk for immunocompromised individuals such as those with AIDS, since resistance to infection is low.
Usually, progression of TB or other mycobacterial infections is slow. But when immunity is weak, as in AIDS, progression can be rapid with death occurring months rather than years. HIV positive individuals, with or without AIDS, are more likely to be infected. Although the pulmonary form of TB is the most well-known to the general public, infection of other organs can occur with both typical and atypical TB. This is more likely when immune resistance is lowered and the bacteria circulate throughout the body. The symptoms of active TB are similar to those of other pulmonary infections—cough, sputum production, night sweats, loss of appetite, weight loss, and fever. Night sweats may also occur with active TB.
Worldwide, tuberculosis is the number two infectious disease killer, accounting for at least two million deaths annually, and two billion people are infected. In the U.S., infection was brought to a very low level with a great public health effort and the discovery of effective medication. However, several circumstances have resulted in an increase in drug-resistant TB in this country. The drug-abuse culture is associated with both poor overall health and poor compliance in taking anti-tuberculosis drugs, even when given freely by public health facilities. Poor compliance in the form of failing to complete treatment regimens has greatly accelerated the emergence of resistance. These are the same individuals most likely to be infected with HIV and share infected needles contaminated with a variety of hepatitis viruses, as well as HIV. The sexually transmitted disease (STD) rate in this group is also much higher than the general population; thus, there is an overall infectious burden decreasing resistance to infection.
Because of the prevalence of drug-resistant TB—as well as other contagious diseases—in immigrant populations from poor countries, public health authorities have a difficult time screening and treating these individuals from the standpoint of numbers. Millions of illegal immigrants have no screening for contagious diseases and represent an even greater public health threat. More than 40% of the population in some countries are infected with TB, including an infection rate of nearly 30% in Latin American countries. One infected person can transmit TB to numerous other individuals, a fact that has been repeatedly documented. Since the number of drug-resistant TB cases in the U.S. is increasing, the number of TB disability claims is likely to also increase unless control is somehow achieved. Drugs currently used to treat TB include isoniazid (INH), rifampicin, ethambutol, streptomycin, pyrazinamide, and others, but their effectiveness is declining. In untreated cases of TB, about half will die within about 5 years; the other half of cases will be split evenly between those who have a spontaneous remission and those who maintain chronic infection.
Multi-drug resistant T.B. (MDR-TB) has a fatality rate exceeding 50%, a factor that should be considered by SSA adjudicators. Extensively drug resistant T.B. (XDR-TB) has an even worse prognosis. However, hope has been found in older antibiotics which were never considered anti-T.B. drugs: meropenem and clavulanate. When given in tandem, these agents have been effective in vitro against all 13 XDR-TB strains tested. T.B. bacteria make an enzyme known as beta-lactamase, which makes it resistant to beta-lactam antibiotics like penicillin and meropenem. Clavulanate inhibits beta-lactamase, so that antibiotics like meropenem can work effectively against the T.B. bacillus. Although human studies are urgently being planned in South Africa and South Korea, the results will probably not be known soon; however, since meropenem and clavulanate are already cleared antibiotics in common use, numerous regulatory requirements that would be required for new drugs have already been satisfied.
History, physical examination, symptoms, X ray and other laboratory data can provide evidence of mycobacterial infection. In advanced stages, TB can produce cavities in the lung. Tuberculous abscesses may be present in any other major organ—brain, liver, kidneys, etc. Most TB claims seen by the SSA involve the pulmonary form. The gold standard for identifying TB is a culture of the micro-organism on an egg-based growth medium, but this procedure can take 4–6 weeks for results. More rapid means of testing are available, such as those using nuclei acid amplification techniques (polymerase chain reaction, PCR), and can provide results in a matter of days. When sputum is coughed up, it is a routine procedure to have it stained to render visible TB bacteria when viewed under a microscope. Reference to the presence of absence of “AFB” (acid-fast bacilli, i.e., mycobacteria) is routinely a part of laboratory examination of sputum coughed up by patients. AFB smears could be done on other material, such as a biopsy of tissue from the lung, when indicated. However, this is merely a screening test and will detect the presence of mycobacteria (which is usually TB bacilli) in only 40–70% of cases. Similarly, a negative skin test for TB, called a purified protein derivative (PPD), does not rule out tuberculosis and less so in immunocompromised individuals such as those with AIDS. While such negative tests are evidence against infection, they are not reasonable proof in clinical medicine of the absence of infection; nor are they acceptable for that conclusion in disability determination. Therefore, the SSA should never quote negative results in such tests as the sole basis of a finding that TB is not present in a claimant.
Other Bacterial Infections
These infections include streptococcus, enterobacter, pseudomonas, yersinia, tularemia, brucella and many others.
Mycotic Infections
There are a number of infections caused by pathogenic fungi that can infect human beings, including histoplasmosis, coccidioidomycosis, coccidioidomycosis, cryptocococcis, blastomycosis, candidiasis, and aspergillosis.
Exposure of the lungs to fungal spores is not normally sufficient to produce infection. Many who are infected remain asymptomatic or have modest acute pulmonary symptoms, and never even see a physician. The situation is different for debilitated individuals, such as those with AIDS, malnourished alcoholics, and those weakened by other chronic diseases or chronic use of corticosteroids. And, of course, a minority of otherwise normal individuals will have severe pulmonary disease requiring aggressive treatment. Without treatment, severe fungal infections can easily be fatal. Fungi are ubiquitous; there is no way to avoid them. For instance, histoplasmosis and blastomycosis spores are prevalent in the soil. Unlike tuberculosis, infection of one person with fungi does not pose a contagion risk to others. Pulmonary infection occurs as a result of inhalation of fungal spores. There are drugs useful in treating severe mycotic infections, such as amphotericin B, itraconozole, fluconazole, and ketoconazole; in patients without immune system compromise, treatment is usually effective. Long-term use of anti-fungal medication is not necessary. AIDS is an exception; after life-threatening infection, maintenance medication is required to prevent recurrence. Generally speaking, modern anti-fungal drugs can be used long-term with minimal toxicity; amphotericin B is potentially toxic, must be administered intravenously, and its use is restricted to a hospital environment for severely ill patients.
Possible symptoms related to pulmonary mycotic infection include fever (which may be low-grade in cases of chronic infection), loss of appetite, weight loss, cough, sputum production, mild night sweats (histoplasmosis), and general malaise. In advanced disease with severe destruction of lung tissue, shortness of breath may be a feature. The diagnosis of fungal infections is usually most accurately done by culture of sputum or other material suspected of being infected. Unfortunately, this is not always possible. For example, the patient might not have enough of a cough to produce samples of infected sputum. Therefore, cultures might be negative despite active disease. Fungal skin tests or tests of the blood are based on immune reactivity; they can be positive without active infection and negative with active infection, so out of clinical context they have little value. Fungal antibody tests can be very helpful, but a significant percentage of positive cases can still be missed. There is no fungal test that can rule out infection with enough accuracy that its results override judgment based on the clinical information. If the treating physician is sufficiently convinced of the presence of active infection that anti-fungal treatment is given, the SSA should generally accept that conclusion. In fact, it is not likely that the treating physician will diagnose a serious fungal infection without information that would also convince the SSA of the reasonableness of that diagnosis. The point is that where there is some question in the SSA’s judgment whether infection is present, that is a “benefit of the doubt” situation and deference should go to the treating source.
Other Fungal Infections
Additional possible fungal infections include mucormycosis, paracoccidioidomycosis, pseudoallescheriosis, sporotrichosis, geotrichosis, and others. With the onset of the AIDS epidemic, fungi that were thought not to infect human beings have become opportunistic upon a weakened immune system. Under the right conditions of susceptibility and exposure, perhaps most fungi are potential human pathogens.
Viral Infections
These infections include adenovirus, cytomegalovirus (CMV), hantavirus, corona virus, respiratory synctial virus and many others.
Parasitic Infections
These infections include amebiasis, toxoplasmosis, malaria, and parasitic worms such as ascaris, stronglyoides, schistosoma, trichinella and others.
Continue to How to Get Disability Benefits for Chronic Persistent Lung Infections by Meeting a Listing.