Aortic Aneurysms
Can I Get Disability Benefits for Aortic Aneurysms?
- About Aortic Aneurysms and Disability
- How to Get Disability Benefits for an Aortic Aneurysm by Meeting a Listing
- Residual Functional Capacity Assessment for Aortic Aneurysms
- Getting Your Doctor’s Medical Opinion About What You Can Still Do
If you have an aortic aneurysm, Social Security disability benefits may be available. To determine whether you are disabled by your aortic aneurysm, the Social Security Administration first considers whether it is severe enough to meet or equal a listing at Step 3 of the Sequential Evaluation Process. See How to Get Disability Benefits for an Aortic Aneurysm by Meeting a Listing. If you meet or equal a listing because of your aortic aneurysm, you are considered disabled. If your aortic aneurysm is not severe enough to equal or meet a listing, the Social Security Administration must assess your residual functional capacity (RFC) (the work you can still do, despite the aortic aneurysm), to determine whether you qualify for disability benefits at Step 4 and Step 5 of the Sequential Evaluation Process.
About Aortic Aneurysms and Disability
The aorta is the largest artery in the body. Receiving cardiac left ventricular blood ejected through the aortic valve, the aorta serves as the source of all systemic arterial blood flow. As it leaves its attachment to the left ventricle, the aorta arches up (ascending aorta) and then downward (descending aorta) until it terminates in the lower abdomen, near the level of the umbilicus, by splitting into the right and left common iliac arteries. In its course, the aorta gives off branches to the various organs and tissue structures of the body. The major branches of the aorta are the coronary, brachiocephalic, common carotid, subclavian, renal, mesenteric, and common iliac arteries. However, aneurysms of these vessels are unusual compared to those of the aorta itself.
As might be expected, rupture of the aorta anywhere along its course is usually fatal. Aortic aneurysms, enlarged and weakened areas of abnormality, present a common and serious medical problem. Rupture of an aortic aneurysm has a 50% mortality rate before the person can reach an emergency room and a 1% per minute increase in mortality in time to treatment. See Residual Functional Capacity Assessment for Aortic Aneurysms.
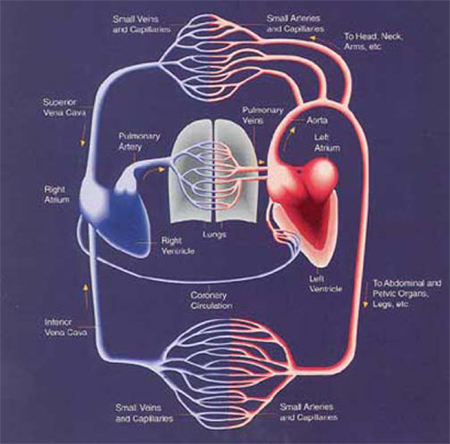
The Cardiovascular System
The normal size of the aorta varies by a number of factors: age, gender, weight, and body surface area. Although men have larger aortas than women, this difference disappears when corrected for body surface area. The aorta also changes size with location, becoming smaller as it descends from the heart.
Since the absolute size of a normal aorta varies, it is better to use a relative measurement rather than an absolute one in making the diagnosis. The most common definition for an aneurysm is when there is a 50% or more increase in aortic diameter; some authorities would also include any increase of at least 3 cm in the definition.
About 80-90% of aortic aneurysms occur below the level of the kidneys and are thus referred to as infrarenal. This reported frequency varies somewhat with different studies. The infrarenal aorta has been reported to average about 1.7 cm in men and 1.5 cm in women after age 50. These numbers could be larger with advanced age; it is important for the clinician to also gauge the normal aortic diameter above the aneurysm to assess prognosis and treatment, rather than the aneurysm alone. If a person has a normal infrarenal aortic diameter of 1.8 cm, he or she would not be considered to have an aneurysm unless there was an area of at least 3.6 cm diameter, and that would be a very small aneurysm. Some studies have classified “normal” as up to 4.0 cm.

A normal abdominal aorta, as imaged by magnetic resonance angiography.
Causes of Aortic Aneurysms
The cause of aortic aneurysms is unknown, although there is a genetic component that contributes to the probability of developing this disorder. A variety of medical conditions can contribute to the development of aneurysms or accelerate their development. For example, the aorta is susceptible to the development of fatty atherosclerotic deposits, and it is not unusual for even very young children to have the beginning of aortic atherosclerosis—probably as a result of the poor, high-fat dietary habits of Americans in general. A degenerative condition affecting the medial layer of the aortic wall is known as cystic medial necrosis, because it damages the elastin (elastic connective tissue) and is thought to be an important contributing factor to the development of aneurysms by weakening the structural integrity of the aorta. Cystic medial necrosis is a feature of several types of connective tissue disorders, such as Marfan’s syndrome. It is also a feature of aging. Trauma can damage the aorta and facilitate development of an aneurysm.
Aortic Aneurysms and Dissection
Aortic aneurysms can undergo a process called dissection, in which blood inside the aorta pushes its way through a tear into the wall of the aorta and splits the layers of the artery apart. Cystic medial necrosis is thought to be important in the development of dissection. Once dissection is present, high blood pressure can accelerate its worsening. When aortic dissection is present, there are several classification systems in use that may be seen in medical records. Aneurysms in the chest area (thoracic aneurysms) are particularly dangerous. A DeBakey Type I aneurysm, for example, could not only involve the aorta but the integrity of the aortic valve and coronary arteries that supply the heart. The longer an aortic aneurysm, the more likely it is to involve major arteries branching to vital organs—such as the renal arteries. The surgical repair of such aneurysms becomes correspondingly more dangerous. For example, a Type I aneurysm that involves the renal arteries can have a 50% operative mortality. Such long aneurysms can be operated, but surgery also carries the chance of paralysis due to compromise of blood flow to the spinal cord, among other risks. On the other hand, discrete and non-dissecting abdominal aneurysms have less than a 2% overall operative mortality.
TABLE 4.10.1.a – 1: CLASSIFICATION OF AORTIC DISSECTION
|
TYPE |
LOCATION OF DISSECTING ANEURYSM |
| DeBakey | |
| Type I | Originates near the aortic valve, involves at least the aortic arch, but may extend the entire length of the aorta. |
| Type II | Originates in and is confined to the ascending aorta. |
| Type III | Originates in the descending aorta (beyond the left subclavian artery) and extends down the aorta. In Type IIIA, the dissection is confined to the thoracic aorta. Type IIIB also involves the abdominal aorta. Rare cases of Type III dissection may extend retrograde into the aortic arch and ascending aorta. |
| Stanford | |
| Type A | All dissections involving the ascending aorta, regardless of the site of origin. |
| Type B | All dissections not involving the ascending aorta. |
| Descriptive | |
| Proximal148 | DeBakey Types I and II or Stanford type A. |
| Distal149 | DeBakey Type III or Stanford type B. |
Surgical Repair
Abdominal aortic aneurysms are frequently encountered in disability claims. In the U.S. alone, there are about 50,000 surgeries for this condition annually. The classical surgery is a midline abdominal incision to acquire access to the aneurysm, which is then opened. A Dacron or similar flexible graft material is then placed in the location of the aneurysm and the aortic walls sewed back around the graft. However, newer and less invasive techniques for repairing abdominal aortic aneurysms are preferable—specifically, the use of endovascular grafts—that have a lower morbidity and mortality for the patient. With an endovascular graft, the patient does not require a large abdominal incision. Instead, a catheter is threaded into the femoral artery in the upper thigh, and is used to insert the graft into the aneurysm area of the aorta. Aneurysms in the thoracic aorta usually involve resection of the diseased part of the artery and replacement with an artificial Dacron conduit. Endovascular prostheses in the form of intraluminal stent-grafts have also been used in thoracic aneurysms with good results. These more advanced and less-invasive surgical techniques will inevitably lessen the overall burden of patient suffering as they become increasingly widespread.
Because of the large numbers of discrete and non-dissecting aortic abdominal aneurysms, there has always been an ongoing medical discussion and many studies about “if” and “when” surgery should be done. The frequency of such aneurysms increases with age, and is present in about 9% of the population over age 65. Male, white, smokers are the group with the highest risk. The normal diameter of the aorta in an average adult is considered to be up to 4 centimeters. Studies have repeatedly confirmed that aneurysms in the 4.0 to 5.4 cm range do not carry sufficient risk of rupture to justify surgery, because earlier surgery does not improve survival. Aneurysm size is the most important determinant of rupture and a size of 5.5 cm is what most authorities would consider needing surgical repair. On average, abdominal aneurysms grow at about 0.32 cm/year and there is a general overall rupture risk of about 0.6%/year. Rapidly enlarging aneurysms, such as those growing 1 cm or more in a year, or 0.7 cm or more in the past 6 months may also be considered operative candidates. In one study, the 1-year predicted rupture rate for 5.5 to 5.9 cm aneurysms was about 9.4%; 10.2% for aneurysms 6.0 to 6.9 cm; 19.1% for aneurysms 6.5 to 6.9 cm; and increasing to 32.5% for aneurysms greater than 7.0 cm in diameter. The 6-month rupture risk for aneurysms of 8.0 cm or larger was 25.7%. Only about half of small aortic aneurysms will increase in size, and those that grow less than 0.15 cm/year have a good chance of never rupturing, while those eventually requiring surgery or which rupture grow at about 0.3 cm/year or more. It should be remembered that, in regard to these risks, there is still no information about how they further correlate with various types of physical activity. It is safe to assume, however, that increasing physical exertion increases the risk—perhaps higher than the risks given here. Tender aneurysms suggest the possibility of inflammation or infection and could also be a reason for earlier surgery. Finally, some patients worry so much about rupture that they would rather take the risk of earlier surgery, although this decision is not logically a good idea.
Not all patients with aortic aneurysms come to surgery. In some cases, medical therapy—especially good control of blood pressure—is preferable in regard to risk. Five-year survival rates of about 75-80% are typical for patients with dissecting and non-dissecting aneurysms, and also in regard to whether there is medical or surgical therapy. It should be remembered that these are overall statistical results. An individual with the repair of a simple aortic abdominal aneurysm will have unlimited functional ability—if they survive surgery—while someone who has not had surgery will still have a risk of rupture. From a disability determination standpoint these individuals are not the same. Cases requiring surgery are those which are immediately life-threatening or carrying a high risk of rupture in the near future—such as progressive dissection involving the arterial branches to vital organs, or the formation of saccular-shaped aneurysms. Chronic and stable dissections in the distal part of the aorta can be treated medically with equivalent survival. Stable aortic arch dissections present difficult surgical problems and may also be candidates for medical therapy.
Continue to How to Get Disability Benefits for Aortic Aneurysms by Meeting a Listing.