Epilepsy
Can I Get Social Security Disability Benefits for Epilepsy?
- About Epilepsy and Disability
- How to Get Disability Benefits for Epilepsy by Meeting a Listing
- Residual Functional Capacity Assessment for Epilepsy
- Getting Your Doctor’s Medical Opinion About What You Can Still Do
If you have epilepsy, Social Security disability benefits may be available. To determine whether you are disabled by your epilepsy, the Social Security Administration first considers whether it is severe enough to meet or equal a listing at Step 3 of the Sequential Evaluation Process. See How to Get Disability Benefits for Epilepsy by Meeting a Listing. If you meet or equal a listing because of your epilepsy, you are considered disabled. If your epilepsy is not severe enough to equal or meet a listing, the Social Security Administration must assess your residual functional capacity (RFC) (the work you can still do, despite the epilepsy), to determine whether you qualify for disability benefits at Step 4 and Step 5 of the Sequential Evaluation Process.
About Epilepsy and Disability
Epilepsy is a disorder consisting of recurrent seizures resulting from some intrinsic dysfunction of the brain. Seizures have many possible forms and, in general terms, can be episodes of alteration of consciousness associated with unusual behavior, sensory experiences, or motor activity. Seizure activity is not necessarily epilepsy. For example, seizures associated with alcohol withdrawal, drugs, toxins, or fever are not considered epilepsy. Such seizures result from abnormal brain physiology imposed by an external factor, rather than being recurrent disorders of intrinsic brain function. The words “seizure disorder” are a non-specific reference to some type of epilepsy, and used when an examining physician does not know the specific type of epilepsy. Epilepsy is common, occurring in about 1% of the population.
The information needed for disability determination includes:
- Detailed description of any aural symptoms.
- Detailed seizure description for each type of seizure, as well as any associated phenomena such as tongue-biting, incontinence, etc.
- Detailed description of the postictal condition of the claimant, including the duration of such phenomena.
- Frequency of seizures per week/month/year, with a clear distinction between the frequency of daytime vs. nocturnal seizures.
- Dates the claimant has been seen in the year prior to adjudication and the number of seizures reported at each visit.
- Date of most recent reported seizure.
- Whether the doctor has personally observed a seizure.
- Type of medication and dosage.
- Statement regarding compliance.
- Blood levels of anticonvulsant drugs, the treating physician’s explanation of any low levels, and evidence to support said opinion.
- Date the claimant was first started on medication.
- Date of last medication adjustment.
- Number of seizures since last medication adjustment.
- Date and results of any electroencephalograms (EEGs).
- Any other relevant medical tests, such as neuroimaging of the brain (CT, MRI).
- Date the claimant was last seen.
- Whether the claimant drinks alcohol and, if so, the amount consumed and whether the physician told the claimant not to drink.
- Detailed history and physical examination.
See Residual Functional Capacity Assessment for Epilepsy.
Causes of Epilepsy
From the perspective of brain physiology and anatomy, the most fundamental causes of epilepsy (epileptogenesis) are still under study. However, two basic brain events must occur together in any clinically significant seizure: (1) hyperarousal and (2) hypersynchronicity. In hyperarousal, large numbers of brain cells (neurons) increase their firing rate—as much as 500/second as opposed to a more normal rate of 80/second. In hypersynchronicity, large numbers of brain cells fire together.
Individuals with congenitally deformed brains often have seizures, and in otherwise normal human brains, there may be an imbalance of inter-neuron signaling chemicals in some area of the brain. There are a large number of such neurotransmitters, but two are particularly important in maintaining normal cortical tone—the proper balance between a mass of brain tissue that is too inhibited or too excitable: gamma-aminobutyric acid (GABA) is generally inhibitory to neuronal activity and glutamate is generally excitatory. Subtle genetic factors may make some people more prone to a neurotransmitter imbalance, or perhaps dysfunction of the small ion channels in neurons that are acted upon by neurotransmitters. A person who does not have epilepsy may be susceptible to developing the disorder with the right kind of trigger.
Basic Neuron Function
Seizures from instigating events such as drugs would not be considered epilepsy because they are both externally imposed on the brain and transient. However, it has been known for many years that brain injury predisposes an individual to the development of epilepsy—whether the brain damage results from an athletic event like football, or from the surgical removal of a brain tumor. In a susceptible brain, the presence of “scar” in the brain can serve as an irritative focus that starts a wave of hyperaroused and hypersynchronous electrical activity in millions of neurons: a seizure. Basically, brain damage makes that organ more susceptible to electrical imbalance and, therefore, seizure activity. For example, epilepsy is more frequent in people with degenerative brain diseases like Alzheimer’s disease, people who have had strokes, infections of the brain, and people with brains invaded by parasitic worms.
Epilepsy may also be associated with cerebral palsy, neurofibromatosis, pyruvate deficiency, tuberous sclerosis, autism, and other disorders. Other triggers can be flickering lights, sleep deprivation, consumption or withdrawal of alcohol, menstruation, antihistamines, antibiotics, anticholinergics, barbiturate withdrawal, methylxanthines, anti-psychotic medication, and or even more exotic causes like certain kinds of music. In fact, flickering light and sleep deprivation are among standard techniques for diagnostic testing during measurement of the brain’s brainwave activity (electroencephalograms, EEGs). About 50–70% of the cases epilepsy are idiopathic—of unknown cause. The onset of new seizures in a previously healthy adult is an ominous sign, and suggests the possibility of a brain tumor that requires immediate investigation.
Finally, there may be some overlap between epilepsy and other types of brain dysfunction. For example, some people with migraine headaches also have epileptic phenomena, a condition that might appropriately be called migralepsy. Some antiepileptic drugs are also effective in the treatment of migraines.
Generalized Seizures
Generalized seizures are those involving widespread neuronal activation in both hemispheres of the brain. Such general brain involvement may result in loss of consciousness, falling, or generalized tonic-clonic activity. Note that the word “generalized” does not refer to the body as a whole, but to the whole brain being affected as opposed to seizure activation of a part of the brain.
Tonic-Clonic Seizures
Most seizures in both children and adults are generalized tonic-clonic seizures (TCS), also known by the older term of grand mal epilepsy. Associated auras (pre-seizure symptoms) characterized by changes in mood or appetite are common in TCS, although wide individual variation is possible. About 75–80% of generalized TCS of unknown cause (idiopathic) can be controlled with medication. The genesis of TCS lies in the neocortex of the brain—the outermost cerebral layer. Secondary generalized tonic-clonic seizures may develop from simply partial seizures or complex partial seizures.
Tonic-clonic seizures are dangerous. Not only is there a risk of status epilepticus (a life-threatening condition characterized by continuous seizures, or repetitive seizures with incomplete recovery between seizures, clinically or electrically on EEG, for period of 30 minutes or more), but also injuries such as head trauma or fractures. Pneumonia may result from aspiration of stomach contents into the lungs. In this latter regard, vertebral body fractures may occur even if there is no direct injury from falling.
Tonic Seizures
There are generalized seizures which are only tonic. In these cases, there are only widespread involuntary muscle contractions without muscle jerking (clonus). There is flexion of the upper extremities, and either flexion of extension of the lower extremities. Injury may occur from falling. Consciousness is usually maintained. Tonic seizures are more common in children, particularly those with generalized epileptic syndromes. The genesis of tonic seizures is probably in the brainstem.
Clonic Seizures
Generalized clonic seizures are rare, and most commonly occur in children who have fever. The genesis of clonic seizures is in the neocortex. First, there is a sudden loss of consciousness followed by either (1) loss of muscle tone (hypotonia) or; (2) generalized tonic muscle rigidity. Then clonic movements manifest as a series of muscle jerks (myoclonus). There are no autonomic nervous system complications and no postictal confusion.
Atonic Seizures (“Drop Attacks”)
A 1–2 second sudden loss in muscle tone is characteristic in atonic seizures. Onset is usually in the 2–5-year-old age range. The whole body may be involved, or just the neck and shoulder muscles with dropping of the head. These seizures are more common in children, in association with various generalized epileptic syndromes, neurological disorders, or mental retardation. The person may fall and be injured, but falling is not necessarily associated with a loss in consciousness. There may be some loss in consciousness, but with quick return to normal within 10–60 seconds.
Myoclonic Seizures
Generalized myoclonic seizures are rapid muscular jerks which can be single or repetitive. The muscular spasms are rapid bilateral, symmetrical and synchronous. In other words, they occur bilaterally in the same groups of muscles at the same time—such as simultaneous contractions in the right and left biceps muscles. However, most spasms are in the face and shoulder muscles. There is no loss of consciousness. This type of seizure most often occurs in children with various forms of epilepsy syndrome.
Absence Seizures
Generalized absence seizures (AS) can be either typical or atypical, and are also known by their older name of petit mal seizures. Absence seizures seem to be related to some type abnormality in the timing parameters of the oscillatory circuits that connect the thalamus in the upper part of the brain stem to the cortex of the brain. The thalamus is important in maintaining awareness; when the thalamus does not electrically pace the cortex properly, awareness is lost.
Coronal View of the Brain
In typical AS, there is a sudden loss of awareness with cessation of whatever activity the person is engaged in performing. These seizures are very brief, usually lasting less than 10 seconds and not preceded by any type of aura. The frequency varies greatly. In severe, untreated cases, hundreds of absence seizures can occur daily. There may be no manifestation in the muscular system—no tonic, clonic, or atonic abnormalities. But some cases have such abnormalities mildly expressed in the eyelids or facial muscles. In some instances, there may also be autonomic nervous system dysfunction or automatisms, but often there is only staring without awareness. Typical AS are frequently associated with generalized tonic-clonic seizures in children who otherwise have no neurological abnormalities. Recovery from a typical AS is usually quick and without residual confusion or other symptoms; the individual is usually not aware that they have had a seizure. Typical absence seizures commonly resolve by late adolescence. Seizures are often inducible by hyperventilation or photic stimulation.
Atypical AS are more likely than typical AS to be associated with other types of brain disorders and mental retardation. There is also a greater likelihood of tonic or clonic manifestations, as well as automatisms (seizure-associated behavior occurring outside of consciousness) like blinking or chewing. Atypical AS are more difficult to provoke with hyperventilation or photic stimulation. The seizure duration is brief, but longer than that of typical AS—most often in the 10–30 second range. Also, entry into the seizure is not quite as abrupt as in typical AS, and emergence into clear consciousness is a little slower.
Partial (Focal) Seizures
Partial seizures are those which have a localized (focal) origin in the brain. Note that the word “partial” does not refer to affecting only a part of the body, but to part of the brain being affected as opposed to seizure activation of the whole brain.
Simple Partial Seizures
Simple partial seizures are those in which there are abnormalities of emotion (affect), cognition (thinking), sensation, autonomic, or motor function without any loss of consciousness. Multiple symptoms can exist simultaneously in simple partial seizures. Memory could be affected, as well as ability to think clearly. However, memory of the seizure itself is intact, and the individual can respond to questions during a seizure. Sensory symptoms could involve taste (gustatory), smell, (olfaction), visual or auditory hallucinations, etc. Motor abnormalities may include involuntary sounds or speaking (vocalizations), or inability to speak. Other motor abnormalities may be involuntary movement of parts of the body, or tonic or clonic activity. The specific types of seizure abnormalities naturally depends on the brain structures involved, as well as the manner and degree in which the epileptic activity spreads.
Some simple partial seizures remain idiopathic, despite the fact that brain imaging techniques can now detect abnormalities that were not visible in the past. The most frequent known cause of the onset of this type of seizure in adults is cerebrovascular disease, which can interfere with normal blood flow to parts of the brain. In children, brain tumors (gliomas) are a common cause of this form of epilepsy, and in adolescents an abnormality of the temporal lobes known as mesial temporal sclerosis can also result in simple partial seizures. Other possible causes include brain tumor in general (benign or malignant), head trauma, and congenital brain deformities. Some people have partial seizures that precede a complex partial seizure, or go on to generalize, i.e., become some type of generalized seizure, including tonic-clonic seizures.
The duration of simple partial seizures is usually less than 30 seconds, and there are no postictal residuals in most instances. In rare instances, there may be some feeling of weakness in an affected limb postictally.
Simple partial seizures may precede generalized tonic-clonic seizures or complex partial seizures. Mental disorders (e.g., panic attacks), migraine headaches, and transient ischemic attacks can produce the same kinds of symptoms and signs as partial seizures so these disorders must be part of the differential diagnostic possibilities.
Complex Partial Seizures
Complex partial seizures are similar to the simple partial seizures described above, except that:
- There is loss of awareness (but no falling) with no memory of the seizure after recovery;
- There may be postictal manifestations (phenomena associated with and occurring after a seizure), such as confusion, lethargy or unusual behavior;
- The typical seizure duration is longer at 1–3 minutes; and
- Abnormal brainwave activity (EEG) is more likely (about 2/3 of cases).
Treatments for Epilepsy
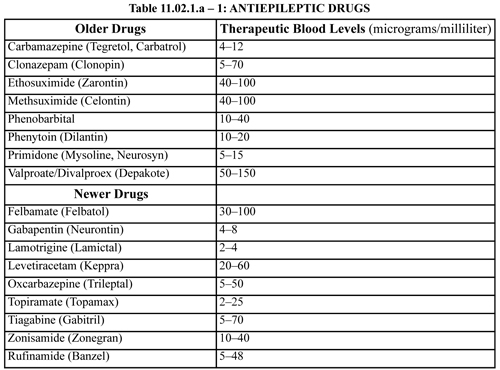
Treatment for difficult-to-control epilepsy may involve brain surgery in the form of cutting the nerve tracts of the corpus callosum that communicate between the two hemispheres of the brain (callostomy), or resection of parts of the temporal, parietal, or frontal lobes to remove a seizure focus. Ketogenic diets are helpful in controlling seizures in some children; it is less effective in adults. Some otherwise intractable partial seizures have responded to implanted pacemaker simulation of the vagus nerve. However, the great majority of cases can be effectively treated with medication. Since the blood levels of antiepileptic drugs (AEDs) are important in determining compliance with prescribed therapy, the generic and trade names of most of these medications is given below, along with therapeutic blood levels. Some drugs do not have an established therapeutic blood level and in others the testing laboratory may differ a little in their normal reference ranges—although not greatly.
Only about one third of patients with a first unprovoked seizure will have further seizures within five years; about three quarters of those with two or three unprovoked seizures have further seizures within four years. Thus, onset of a single partial or general seizure is never treated even if it is otherwise compatible with some type of epilepsy. However, about three-fourths of those who have a second unprovoked seizure will have further seizures within four years. The more seizures that occur, the higher the probability that there will be additional seizures. Therefore, treatment should be started after the second seizure.
Unfortunately, many claimants seen for SSA disability evaluation remain on older drugs. However, the newer drugs can not only achieve seizure control but decrease cardiovascular and stroke risk factors. Thus, it is questionable that anyone be started or maintained on the older agents, unless there has been treatment failure with newer agents. However, SSA has no control over treating source prescribing practices and cannot hold the result of less-than-optimal practices against the claimant at adjudication.
Continue to How to Get Disability Benefits for Epilepsy by Meeting a Listing.