Breast Cancer
- About Breast Cancer and Disability
- How to Get Disability Benefits for Breast Cancer by Meeting a Listing
- Residual Function Capacity Assessment for Breast Cancer
- Getting Your Doctor’s Medical Opinion About What You Can Still Do
Can I Get Social Security Disability Benefits for Breast Cancer?
If you have breast cancer, Social Security disability benefits may be available. To determine whether you are disabled by your breast cancer, the Social Security Administration first considers whether it is severe enough to meet or equal a listing at Step 3 of the Sequential Evaluation Process. See How to Get Disability Benefits for Breast Cancer by Meeting a Listing. If you meet or equal a listing because of your breast cancer, you are considered disabled. If your breast cancer is not severe enough to equal or meet a listing, the Social Security Administration must assess your residual functional capacity (RFC) (the work you can still do, despite the breast cancer), to determine whether you qualify for disability benefits at Step 4 and Step 5 of the Sequential Evaluation Process.
About Breast Cancer and Disability
Although breast cancer is principally a cancer of women, it occurs in men at 1% the frequency it is found in women. Treatment and prognosis in men is similar to that for women. The highest incidence of breast cancer is after age 65. The annual mortality has not changed over past decades, despite all the efforts of medicine and has remained fairly constant as a cause of death in 27/100,000 females. There is approximately a 10% cumulative risk for a woman to develop breast cancer during her lifetime.
At the time of diagnosis, about half of the patients already have spread of cancer to the axillary regional lymph nodes. The most frequent sites of distant breast cancer metastases are lymph nodes, lung, bone, liver, adrenal glands and skin. However, any organ could be involved. To expect cure of breast cancer, all cancer would have to be captured by the initial surgery and this does not happen unless the cancer is detected very early.
Recurrent cancer is more likely with larger primary tumors and if there was cancer in the axillary lymph nodes at diagnosis. For example, a patient with a small tumor less than 2 centimeters in diameter and negative axillary nodes will have a 5-year recurrence rate of about 10%, but over 20% if the tumor is greater than 5 centimeters. A small tumor with positive axillary nodes has a recurrence rate of about 50% at 5 years, but large tumors positive axillary nodes will be associated with recurrent cancer in about 65 – 75% of cases at 5 years.
The SSA must be able to obtain all necessary pathology reports showing that breast cancer is present. See Residual Functional Capacity Assessment for Breast Cancer.
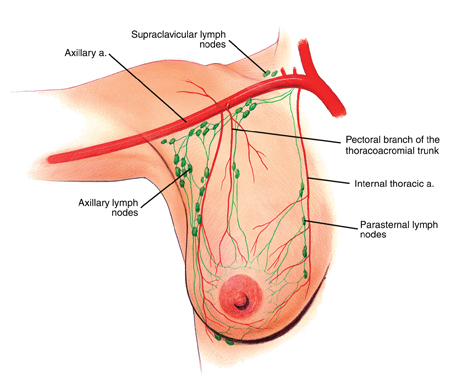
Blood Vessels and Lymphatics of the Breast
Types of Breast Cancer Tumors
There are many possible tumor types. Infiltrating ductal carcinomas are the most frequent, accounting for over half the cases. If the nipple is involved with crust, burning, oozing or bleeding in association with an underlying carcinoma, then the term Paget’s disease is used. This is not a separate form of cancer and treatment is the same as for other breast cancers. Approximately 6% of breast cancers are medullary carcinomas, which have a better prognosis than intraductal carcinomas. Tubular and mucinous carcinomas of the breast also have a better outcome than infiltrating ductal cancers. Infiltrating lobular carcinomas account for up to 10% of breast cancers.
TNM System of Breast Cancer Staging
The TNM staging system is sometimes used to describe the extent of breast cancer in a patient’s body. T1-T4 denotes the severity of the primary cancer, with T4 being the worst. T1 tumors are 2 cm or less in diameter; T2 tumors are more than 2 cm, but not more than 5 cm; T3 tumors are more than 5 cm. T4 tumors are of any size that involves the chest wall (ribs or muscles between the ribs) or skin. There is a further a and b sub-classification. T1a-T4a tumors are not fixed to the underlying connective tissue or muscle. In T1b-T3b lesions, there is such a fixation. T4b involves ulceration of breast skin, satellite skin nodules in the same breast, or edema of the breast. T4c is a combination of T4a and T4b. T4d refers to inflammatory carcinoma.
N0-N3 denotes the degree of regional lymph node involvement. N0 means no palpable axillary (armpit) lymph nodes on the same side as the involved breast; N1 means there are movable axillary nodes on the same side as the involved breast; N2 means positive axillary nodes on the same side as the involved breast that are fixed to each other or other structures; N3 means there are positive nodes below or above the clavicle, or edema of the arm. M0-M1 describes metastatic disease. M0 means there is no distant metastasis. M1 refers to distant metastasis.
In addition, there is a clinical Staging I-IV. Any T4, N3, or M1 tumor is Stage IV. Early cancers with no axillary lymph node invasion are Stage I. Stages II and III are various combinations of more advanced primary tumors and lymph node metastasis. About 50% of cases have spread to axillary lymph nodes. About 80-90% of Stage I tumors will survive 5 years. This drops to about 65% for Stage II, 40% for Stage III and 0% for Stage IV.However, various studies report a wide range of survival rates dependent on tumor type, stage, and treatment. Nevertheless, it is clear that distant metastasis is generally incurable and will result in death within several years in most cases.
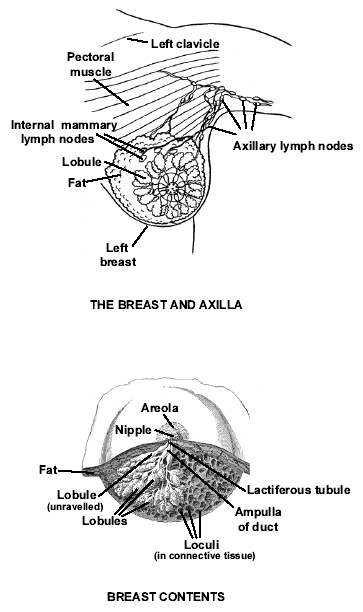
Anatomical Drawings of the Breast
Breast Cancer Treatment
Surgery, radiation, endocrine therapy, and chemotherapy are all used in various combinations in the treatment of breast cancer. The advanced but still operable lesions require a radical mastectomy, which means removal of the breast and underlying pectoralis major and minor muscles of the chest, as well as the axillary lymph nodes. A modified radical mastectomy is similar, but spares the largest chest muscle, the pectoralis major. Some early cancers can be treated with simple (total) mastectomy, which involves removal of the breast alone. The most conservative and breast preserving surgery (lumpectomy) can be done on selected very early cancers.
Some breast cancers have receptors on the malignant cells which respond to estrogen or progesterone, and their growth is accelerated by these hormones. It is possible to assay breast cancer tissue removed at surgery to determine if such receptors are present. If so, endocrine therapy can be of some benefit. Tamoxifen is a drug of low toxicity that produces relatively few side effects, and it is an anti-estrogen agent that acts by occupying the receptor sites on cells that would otherwise be available to estrogen. It is most frequently used in postmenopausal women. It may even have some value in cancers without estrogen receptors, and this is under investigation. The use of Tamoxifen has largely supplanted other endocrine treatments, such as ablation of the ovaries.
Chemotherapy is given after surgery in those cases with regional lymph node involvement or worse. Various drugs have been used for their cytotoxic effects on breast cancer cells. These drugs are toxic to the patient, as well as to the cancer. For example, doxorubicin can damage heart muscle, and vinblastine can be toxic to peripheral nerves. Response to chemotherapy is not immediate; several months are usually required to see improvement, if there is going to be any. Patients who have already had chemotherapy or radiotherapy, or who have metastases to bone or liver are less likely to respond as well.
Radiotherapy can reduce the incidence of local recurrence at the chest wall mastectomy site or in the regional lymphatics, but does not appear to confer additional benefit in survival. The reason for this is that distant metastatic disease may have already occurred and kills the patient. Nevertheless, local recurrences are distressing, and radiation to the mastectomy site or regional lymphatic vessels is sometimes given after chemotherapy. In addition, solitary metastatic lesions might be treated with radiation, such as painful metastasis to a vertebral body. It is also used to treat metastatic lesions to the central nervous system (brain or spinal cord).
Continue to How to Get Disability Benefits for Breast Cancer by Meeting a Listing.