Kidney Damage
How to Get Disability Benefits for Kidney Damage by Meeting a Listing
To determine whether you are disabled at Step 3 of the Sequential Evaluation Process, the Social Security Administration will consider whether your kidney damage is severe enough to meet or equal the kidney damage listing. The Social Security Administration has developed rules called Listing of Impairments for most common impairments. The listing for a particular impairment describes a degree of severity that Social Security Administration presumes would prevent a person from performing substantial work. If your kidney damage is severe enough to meet or equal the listing, you will be considered disabled.
The listing for kidney damage is listing 6.02, which has three parts, A, B, and C. To meet the listing you must satisfy any of the three parts. To satisfy any of the three parts of the kidney damage listing, you must have impairment of renal function due to any chronic renal disease that has lasted or can be expected to last for a continuous period of at least 12 months.
Meeting Social Security Administration Listing 6.02A for Kidney Damage
You will meet listing 6.02A if you have chronic hemodialysis or peritoneal dialysis. A report from an acceptable medical source describing the chronic renal disease and the need for ongoing dialysis is sufficient to satisfy the requirements in this listing.
Keep in mind that part A is satisfied only when dialysis actually begins for chronic renal failure. The permanent surgical shunts that are placed in a patient’s wrist by creating a fistula (opening) between the radial artery and a native vein take time to heal (6–12 weeks) and may be done as long as 6–12 months before dialysis actually starts. There are also prosthetic (“graft”) arteriovenous shunts that take about 3–8 weeks to heal. Therefore, placement of a shunt cannot be used as evidence of dialysis satisfying part A. However, by the time a shunt is placed, part C will often (but not necessarily) be satisfied.
Meeting Social Security Administration Listing 6.02B for Kidney Damage
You will meet listing 6.02B if you have undergone a kidney transplant. After transplantation, there are numerous possible complications, so part B recognizes the need of a year for post-operative recovery. Claimants are an unqualified allowance under part B for a full 12 months post-transplantation, even if the treating physician states they are well enough to return to work before then.
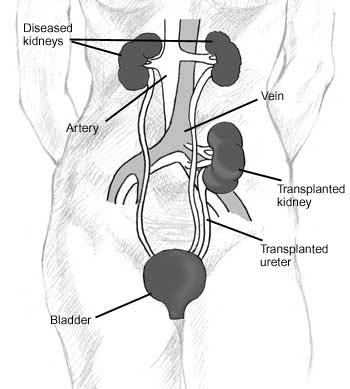
Position of Transplanted Kidney
Meeting Social Security Administration Listing 6.02C for Kidney Damage
You will meet listing 6.02C if you have persistent elevation of serum creatinineto 4 mg. per deciliter (dL) (100 ml.) or greater, or reduction of creatinine clearance to 20 ml. per minute (29 liters/ 24 hours) or less, over at least 3 months.
Serum creatinine (S. Cr.) refers to the blood level of a chemical called creatinine. It is normally filtered out by the kidneys, so if there is severe kidney disease the amount of creatinine in the blood will increase. This laboratory test gives doctors a good measure of kidney disease severity and only requires a simple blood test. Normal values are less than about 1.5 mg%. Part C requires that the value be at least 4.0 mg% or higher. Alternatively, the creatinine clearance (Cr.Cl) can demonstrate poor kidney function if not over 20 ml/min, which specifies how many milliliters of blood per minute are cleansed of creatinine. The creatinine clearance requires collection of both urine and blood samples. Normal creatinine clearance values are 130 ± 20/ml/min in males and 120 ± 15 ml/min in females. The lower normal values for women favor them over men in regard to qualifying under Part C, but that is the way SSA wrote the listing. For either S. Cr. or Cr. Cl, abnormalities must be demonstrated on repeated blood tests for at least 3 months before any of Part C’s subsections can be used.
Part C has four subsections, numbered 1 through 4. To meet the listing you must satisfy any of the four subsections.
Part C.1
You will meet part C.1 if you have any one or combination of four abnormalities that may be seen with chronic renal failure: osteitis fibrosa cystica, osteoporosis, osteomalacia, or pathologic fractures. Osteitis fibrosa cystica is a fibrous degeneration of bone with cysts. In osteoporosis, there is a loss of bone mass. Pathologic fractures are breaks in bone that occur without trauma or with minor trauma that would not fracture normal bone, and are particularly likely in the structurally weakened bone of osteoporosis and osteitis fibrosa. Plain X-rays of bone are sufficient to establish a diagnosis, but that does not mean a normal plain X-ray implies normal bone. Bone densitometry is non-invasive and much more sensitive than plain X-rays in detecting osteoporosis. This fact should be kept in mind if the SSA adjudicator tries to equate normal plain X-rays with the absence of osteoporosis. The SSA is easily capable of purchasing bone densitometry. Because of the substantial possibility that bone disease is present in anyone with chronic renal disease whose serum creatinine has progressed to 4 mg/dl or higher, the SSA adjudicator should not assume that bone abnormalities are absent, just because the medical records are silent on that possibility.
Similarly, a statement by the treating physician that bone disease is not present has no value if that physician has done no testing and therefore does not actually know whether there is bone disease or not. One must beware of tricky statements by the SSA adjudicator or treating physician such as: “There is no evidence of bone disease,” or “There is no diagnosis of bone disease.” Such statements do not establish the absence of bone disease without clarification of how such conclusions were reached.
Part C.2
You will meet part C.2 if you have persistent motor or sensory neuropathy, and the clinical record must show that the neuropathy is a severe impairment that has lasted or can be expected to last for a continuous period of at least 12 months.
Motor nerves which stimulate muscle contraction necessary for any movement and sensory nerves which permit the various kinds of sensation can both be damaged by severe kidney disease. Numerous metabolic abnormalities are present in chronic renal failure (CRF) and these abnormalities affect nerve function in ways that are not fully understood. Diabetes mellitus is frequently present in chronic renal failure, because it is the most common cause of kidney failure. Diabetes is a major cause of neuropathy, even when there is no kidney disease, so that disorder is an added risk factor for neuropathy. Part C.2 does not require a specified degree of severity, or say how the neuropathy must be demonstrated.
Neuropathy is most easily and specifically diagnosed with a nerve conduction velocity study (NCVS), and the SSA is certainly capable of purchasing such testing if it is not available from the treating physician. However, it should also be sufficient that physical examination data show the clear presence of neuropathy. For example, motor peripheral neuropathy can produce muscle weakness, decreased reflexes, and even muscle atrophy. Sensory peripheral neuropathy is usually in a glove-stocking distribution. In other words it tends to affect an entire hand and fingers, as the fitting of a glove; or in the lower extremities the sensory abnormalities are generalized as would be the fit of a stocking. This is an important medical fact, because peripheral sensory neuropathy does not have to follow an anatomical distribution as it would if a herniated disc (HNP) were pressing on a nerve root, and the SSA adjudicator might not know the difference.
Sensory peripheral neuropathy symptoms are characteristically abnormal sensory perceptions (paresthesias), particularly numbness (hypoesthesia) and a burning pain (burning dyesthesia). Sensory neuropathy usually starts earlier in CRF than motor neuropathy. NCVS are usually used to monitor progression of neuropathy, and the beginning of neuropathy is actually a signal that dialysis should be started. Dialysis will usually (but not invariably) produce a fast improvement in the renal component of neuropathy, i.e., that not caused by diabetes.
Part C.3
You will meet part C.3 if you have persistent fluid overload syndrome.
When kidneys are severely diseased, they can no longer filter out extra water from the body efficiently. Increased fluid in the vascular system can then cause the blood pressure to increase. If the diastolic blood pressure is 110 mm Hg or higher, then part C.3 can be fulfilled. It should be emphasized that the high diastolic blood pressure of 110 must be due to fluid overload from kidney disease. However, many people with renal disease have pre-existing hypertension and others develop hypertension as a result of the renal disease which is not a result of fluid over-load. These possibilities can make it difficult to determine if hypertension is caused by fluid over-load, but the benefit of any doubt should go to the claimant. Blood pressure readings in longitudinal medical records can be most helpful, as well as the degree of renal disease severity. Clearly, mild renal disease is not going to produce hypertension as a result of fluid overload.
Another way to satisfy part C.3 is by signs of vascular congestion. Vascular congestion means signs of abnormal fluid accumulation on physical examination by a doctor, such as swelling of the feet, arms, or face, or other findings (such as a pulmonary edema on a chest X-ray, or an enlarged liver) that excess fluid is present in the body. Signs of vascular congestion are the most observable means of determining whether there is a fluid overload syndrome as the cause of hypertension, yet part C.3 by its wording makes it possible to be allowed with fluid overload syndrome and vascular congestion without hypertension. If dialysis is performed correctly and with sufficient frequency, and the claimant is compliant with prescribed therapy, then persistent fluid overload is not something that would be expected to occur.
Part C.4
You will meet part C.4 if you have persistent weight loss determined by body mass index (BMI) of less than 18.0, calculated on at least two evaluations at least 30 days apart within a consecutive 6-month period.
Continue to Residual Functional Capacity Assessment for Kidney Damage.
Go back to About Kidney Damage and Disability.